Francis Dixon says the City of Ottawa’s shift toward person-centred care has enhanced his sense of independence and dignity at Carleton Lodge, a long-term care home by the Rideau River — one of four run by the city.
“I can wake up when my body allows, and the staff genuinely care about my needs,” the 87-year-old retired clergyman told Capital Current.
Dixon says he finds comfort in the personal touches — from choosing his own wake-up time to swapping a plastic cup for a ceramic one — small changes that make a big difference.
Recently, the City of Ottawa expanded the program, called the ‘person-centred care’ model, which gives residents more autonomy. This model is integrated in all four of the city’s long-term care homes.
Before implementation, Dixon says his days were dictated by a set routine. Now, he enjoys the freedom to wake up and eat according to his own schedule.
“I was sitting at the dinner table today at noon eating a beautiful meal of chicken with a delicious salad and vegetables and I thought to myself again, how very fortunate I am to have people who prepare such a beautiful meal and then staff who serve up so beautifully,” Dixon said.
Dixon, who served with the Salvation Army for 41 years, said he has learned to play bingo and enjoys musical and other social events at Carleton Lodge.

Bay Ward Coun. Theresa Kavanagh, who is also council co-liaison for older adults, explained that person-centred care has led to better mobility, cognitive stimulation, higher job satisfaction for staff and better resident engagement.
Delayed by the pandemic, Kavanagh said the initiative is now being fully implemented, creating a home-like environment with flexible mealtimes and personalized care.
“It was not possible to implement person-centred care under strict rules during the pandemic,” she said. “This model allows care plans tailored to the preferences of residents, ensuring they were more engaged in activities they enjoyed. This approach has so far led to increased mobility and cognitive stimulation of residents.”
Community concerns about dementia care while providing individualized, respectful care, she said, inspired the implementation of a person-centred care model in long-term care facilities.
She said funding for this program comes from the province and the goal is to improve quality of life and prevent unnecessary long-term care admissions by promoting social and physical activity among seniors.
Sheila Bauer, the city’s long-term care administrator, acknowledged the challenges in shifting to this new care model, including cultural change and the need for specialized staff training.
“I would say there is a positive opportunity for change. Understanding that this work involves a cultural change in relation to an approach to care is the essence of the challenge,” she said.
Bauer said transitioning from a rigid, task-oriented approach to a more resident-focused, emotionally based care model — incorporating feedback from staff, families, and external agencies — makes it person-centred.
Despite the hurdles, residents are benefiting emotionally and physically, with improved health outcomes and more engaging daily activities.
She said the metrics for measuring the success of person-centred care include quality-of-life indicators, safety, and staff engagement. For instance, one positive outcome includes personalized dinning experiences and accommodating residents’ preferences, such as natural wake-up times.
A vision for future care
Linda Garcia, professor and director of the LIFE Research Institute at the University of Ottawa, emphasized the importance of creating dementia-friendly environments and accessible spaces for seniors.
Garcia, who has researched how different environments affect the quality of life of individuals with neurological disorders, lauded the person-centred approach as meaningful.
“The physical environments, social interactions, and societal regulations influence seniors’ well-being,” she said, emphasizing the importance of accessible environments, dementia-friendly settings, and changing societal attitudes toward aging.
Garcia said challenges with this model include resource constraints and the necessity of specialized caregiver training. But she remains hopeful about the future of person-centred care.
“I’m optimistic about the younger generation’s push for individuality and tolerance. This kind of attitude will create room for understanding and accommodating individual needs in care settings,” she said.

Anna Lyall, a retired teacher who volunteers in the tuck shop at Carleton Lodge, says she has witnessed how personalized care enhances the lives of residents, especially those with cognitive challenges.
“It is about considering individual preferences and needs, taking into account the resident at the centre of care as well as other aspects of living in a long-term setting,” Lyall said.
Lyall adds that the caregiver in this home takes into cognizance the residents’ preferred activities, whether in a small setting, by themselves or in a large group, allowing them to make their own choice is empowering.
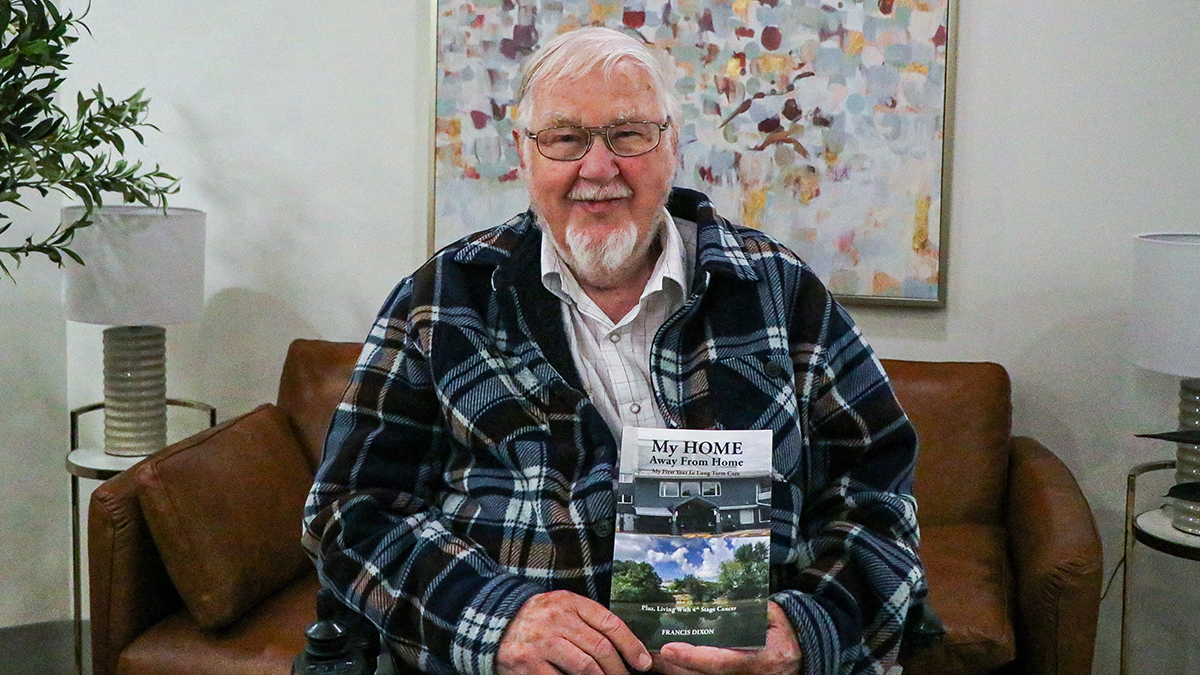
Meanwhile, Dixon is excited to continue pursuing his writing hobby, with two more manuscripts in the works, making new friends, and positively impacting lives while he can.
Dixon’s recently released book titled “My Home Away from Home,” tells the story of his one-year journey to being in a care home, his adaptation to his new life, and his activities. He says he looks forward to more happy moments.
“The experience has been worthwhile, and I feel fulfilled.”