Before Ashley Graham goes into work in the morning, she is sure to finish her coffee along with a bottle of water. She will be wearing a surgical mask for the next few hours, and won’t be able to eat or drink until lunch.
“We get one mask per day,” Graham said, “so usually I try to limit the times I’m taking it off.” Touching and taking off the mask, she said, presents the highest risk of contamination.
Graham is a pharmacist at Women’s College Hospital in Toronto, a facility that has a COVID-19 assessment centre but does not directly treat COVID-19 patients. That said, the increased risk of infection in any hospital setting means that all staff must now wear basic personal protective equipment, or PPE. This equipment is essential to protect health care workers and patients alike, but wearing it for prolonged periods can have other ramifications on people’s day-to-day health.
“It’s not full PPE,” Graham said, “but it’s a lot more than I’m used to wearing.”
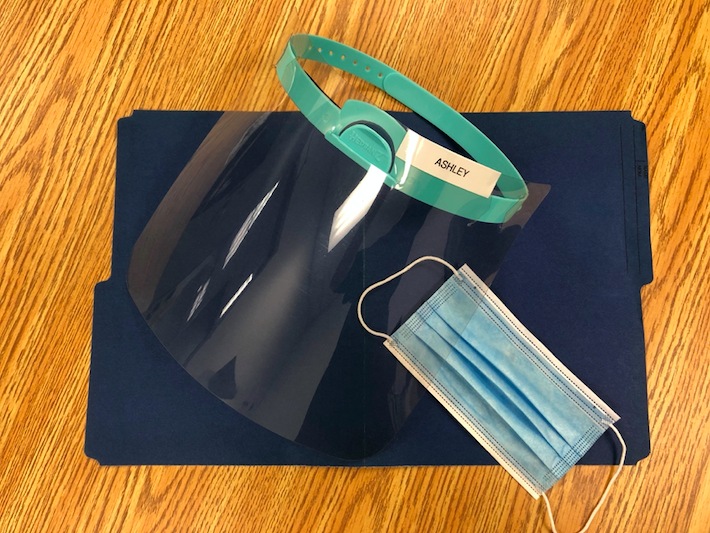
Upon entering the hospital every morning, Graham is faced with a number of screening questions concerning travel and potential symptoms. After answering the questions, she is given a surgical mask for the day. She then heads to the floor that she works on and changes into scrubs. Whenever she enters a patient-care area, she wears a plastic face shield over her mask for added protection.
“I’m usually just wearing my regular work clothes throughout the day,” she said, referring to her pre-COVID-19 routine. “We’d put on PPE on a case-by-case basis,” she added, which wasn’t necessary for most interactions with patients.
Since COVID-19 can be spread through coughing and sneezing, all staff and patients are now required to wear masks in public spaces throughout the hospital.
“You’re not able to drink a lot of water because you have the mask on,” Graham said, “so you can’t take those sips you’re used to taking throughout the day.” She said that she only takes her mask off at lunch, the only time to eat, drink and breathe freely during her shift.
“It’s really hard to get used to wearing a mask all day,” Graham said. “You’re breathing in your own air. I often feel a bit short of breath. I take the stairs at work, but it’s a lot harder with a mask on.”
“Everyone has been feeling a bit more tired. The 3 o’clock slump is a lot more pronounced.”
– Ashley Graham, Pharmacist
She said wearing the face shield for long periods of time also presents new challenges.
“It’s sometimes difficult to read a computer screen, because you have glare and blurriness,” she said. “And I think the most difficult thing is actually hearing your colleagues. We’re yelling all day, because everything kind of muffles what you’re saying.”
Graham said communicating like this expends energy, taking a particularly heavy toll when caffeine and water are unavailable throughout the workday.
“I think everyone has been feeling a bit more tired,” she said. “The 3 o’clock slump is a lot more pronounced. I’m prone to headaches, and so I’ve found that this has been a bit of a trigger for that, as well.”
Communicating with patients is also more difficult, she said, with PPE masking most facial expressions. “Many people, including myself, get enjoyment from connecting with patients,” she said. “And there’s this extra barrier now.”
Holly Rector, a nurse practitioner at the WCH’s cardiology clinic, has faced similar difficulties with the increase in PPE.
“Before COVID, there really wasn’t any PPE at all,” she said. Workers would regularly disinfect equipment and wash their hands, but masks and face shields weren’t necessary for most interactions.
“Your mask gets moist, kind of uncomfortable to wear.”
Holly Rector, Nurse
Like Graham, Rector gets a new mask every morning when she enters the hospital. That said, if the mask tears or gets dirty throughout the day, staff can always get another one.
Rector also has a face shield for interactions with patients, which she regularly disinfects. “All the material on it is plastic,” she explained. “So it can be wiped down.”
She said constantly wearing PPE has affected when she eats and drinks during the workday.
“I would say across the board, all of us have noticed that we definitely don’t drink as much water when we’re wearing our masks,” she said. “I drink more water now at lunchtime – it’s an hour where I focus on getting hydrated.”
Rector, who is 24 weeks pregnant, also finds it more difficult to walk up the stairs in a mask. Physical distancing measures allow for only two people to ride the elevator at a time, so many take the stairs. But Rector explained that PPE makes the climb all the more difficult.
“Your mask gets moist, kind of uncomfortable to wear. I might need a few more breaks on the way up,” she said. “It does take a bit longer to recover wearing the mask.”
These days, Rector has limited contact with patients to avoid exposure to the virus. However, she said that many nurses in the cardiology clinic are still testing patients, and need to wear much more than just face coverings.

Preeya Hanmiah, a respiratory therapist in a Hamilton hospital, is intimately familiar with these additional layers of protection, since she deals directly with patients experiencing breathing problems. Working in a variety of units throughout the hospital, Hanmiah often carries a backpack loaded with all the PPE she might need to respond to emergency situations.
“It takes a few minutes,” she said, referring to the process of putting on the equipment, “which is a huge deal when you have a patient that’s ‘vital signs absent’.”
Before COVID-19, Hanmiah said that protective equipment would only be necessary for certain high-risk procedures, such as intubation, the first step for putting someone on a respirator. These days though, things are different.
Now she is screened at the hospital entrance, where she receives an envelope containing two surgical masks. She has to put one on as she enters the hospital, and wear it in any public or patient-care areas.
The amount of PPE Hanmiah wears depends on the procedure. If she’s intubating a COVID-19 patient, however, she dons full protective gear.
“There’s five pieces that you wear,” she said.
“You can’t see your friends walking by because you can’t recognize them with a mask on their face. The only expression you see is the eyes now.”
– Preeya Hanmiah, Respiratory Therapist
It starts with an N95 mask, followed by a white hoodie that covers the shoulders and head, fastening beneath the chin to stay tight against the face. Then there’s a face shield with a flap extending under the other material, leaving no skin exposed. Finally, there’s a yellow gown that goes on top, with the sleeves tucked into latex gloves.
For certain procedures, Hanmiah — along with other members of a medical team — wear full PPE for hours.
“Communication can be a problem, because you really have to speak up,” she said. “Your ears are completely covered, your mouth is completely covered. Another huge thing is fog. Breathing can fog up your shield so easily.”
The full PPE, combined with the stress of these situations, often makes things physically difficult. “You are perspiring unbelievably. A lot of people come back out drenched in sweat,” Hanmiah said. “It takes a toll on you.”
She added that it is common to feel faint in these situations, especially for colleagues who were fasting during Ramadan.
Bathroom and water breaks are only possible once the work is done and all PPE is removed.

“You have to take it off in a certain order,” Hanmiah said, explaining that discarded equipment can contaminate the hands or face. The routine includes a hand wash after each component is taken off.
Hanmiah also said that wearing a mask all day can irritate the skin behind your ears, where the strap sits for hours. Wearing the N95 mask for long periods of time hurts the bridge of your nose as well, since the mask is pinched by an adjustable aluminum clip.
“You get marks all over your face wearing this stuff,” she said. “You’re sweating, it’s hot, and it has to be tight on your face. You’re noticing things like pimples a lot more, too.”
The physical challenges also come with social ones.
“The demeanour, the rapport, everything’s changed a lot amongst colleagues,” said Hanmiah. “You can’t see your friends walking by because you can’t recognize them with a mask on their face. The only expression you see is the eyes now.”
As a result, it can feel like there are certain barriers between colleagues at work, Hanmiah added.
“It has a lot of social and psychological implications that people don’t realize.”





[…] A look at the side effects of wearing personal protective equipment […]
[…] The price of protection: The physical toll of PPE on health care workershttps://capitalcurrent.ca/the-price-of-protection-the-physical-toll-of-ppe-on-health-care-workers/ […]