Healthcare practices have arguably been the most affected by the last seven months of chaos caused by COVID-19.
In their work on the front lines, they have had to change protocols to keep patients, families and staff safe from the virus. Hospice care, though often overlooked, has also experienced these transformations to stop the spread of COVID-19 — at a cost.
Hospice care focuses on providing end-of-life comfort for people with terminal or life-limiting illnesses that mean the patient or the patient’s family have become unable to care for them.
Comfort and quality of life are the main goals for nurses and personal support workers taking care of residents living in a hospice or patients living at home getting palliative care.
According to the Canadian Hospice Palliative Care Association 2020 report, one in six Canadians used publicly funded hospices between 2016 and 2017.
About 80 per cent of palliative care patients begin receiving comfort care in hospitals or acute care centres before being transferred to a hospice house for palliative care.
Canadians aged 45 to 74 are the largest age group receiving palliative care, placing them above older seniors and younger adults, according to the CHPCA study.
There are three hospice houses in Canada’s capital operated under the charitable organization Hospice Care Ottawa. The HCO runs two residential homes — May Court Hospice located in Old Ottawa South and Ruddy-Shenkman Hospice in Kanata. The organization also operates a day hospice, Le Maison de l’Est, in Orleans — a francophone facility where patients can participate in activities for social interaction and support therapies, among other things.
Lisa Sullivan, the executive director of Hospice Care Ottawa, said that because of the pandemic, hard decisions had to be made this year about the care they could safely offer.
“Our goal when COVID hit was to maintain the services in the residence — that’s the people who are at end-of-life. We had to put a pause on our (in-person) community program,” said Sullivan. “For most of our community programs we maintain contact with our clients in the community either by phone or computer and have been trying to run some programs virtually, such as webinars, meditation sessions or yoga sessions.”
However, resident and patient care cannot be stopped or be transferred to a virtual environment, causing a ripple of changes across Canada for those involved in end-of-life care.

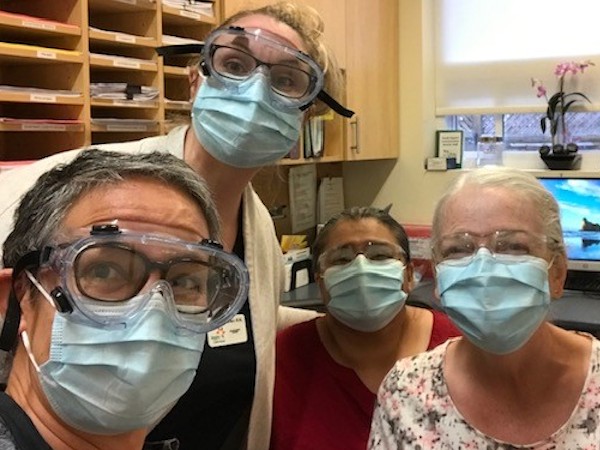
when caring for a new resident. (Photo courtesy Lisa Sullivan)
New protocols in hospice houses include strict limits on visitors, full personal protective equipment (or PPE) for staff and COVID-19 screening for staff and essential visitors.
PPE keep nurses, personal support workers, residents and their families safe. But staff have noticed that protective masks create a barrier between the resident and those delivering the personal care.
Required PPE for a new resident generally is full gown, eye protection, face shield, mask and gloves. At Hospice Care Ottawa, once a patient has received a negative test result, the nurses and PSWs wear just eye protection and masks.
Across the province, protocols can vary somewhat. At McNally House Hospice in the Niagara Region town of Grimsby, executive director Pamela Blackwood said once new residents have tested negative before coming into the hospice and passed the mandatory isolation of between 10 and 14 days, caregivers wear only a mask.
“It’s really hard to get close to people when you have all (the PPE on) to feel like you’re connecting and communicating with someone. Most of our staff have taken a picture of themselves and they hang it on their name tags so that people can see what they actually look like without all of it on,” said Sullivan.
Back in the early days of the pandemic, PPE for hospices was hard to come by.
Hospice Care Ottawa waited until May to get a steady flow of PPE, Sullivan said. Blackwood said McNally House waited until about July.
“Unfortunately the suppliers in Ontario at the beginning were only moving their supplies to hospitals . . . so we were purchasing off of Amazon, anywhere local we could find them, and then we put an appeal out to our community,” Blackwood said.
Blackwood said the Grimsby and broader Niagara community did rally around their hospice, giving donations that included water-proof ponchos from Niagara Falls’ Hornblower Niagara Cruises.
Another major issue has been the restriction of visitors for terminally ill residents, normally an important part of providing compassionate care.
“I think one of the key ways that institutions and health professionals can provide compassionate care is to really stay attuned to the human story, the human aspect,” said Dr. Steven Bellemare, the director of practice improvement at the Canadian Medical Protective Association.
“The whole process of accompanying the patient at the end of their life is very much centred around friends and families being able to congregate to say their last goodbyes and with visitation limitations, (now) that’s often not possible,” said Bellemare.
Hospice Care Ottawa is allowing three essential visitors for their residents, but with the growing number of cases in Ottawa, even that could change at any time.
“(Families) understand that and they want to protect their loved one, and they want to protect themselves,” said Sullivan. “But I think a lot of families, especially large families, it’s really hard for them to understand why they can’t have everyone in and that’s really tough.”
Virtual, garden and window visits provide another option to say goodbye to a loved one while not being permitted inside a facility as one of a patient’s three essential visitors.
At McNally House Hospice, Blackwood said they are experiencing similar challenges. However, because they are not in a provincial pandemic hotspot, each patient is allowed five essential visitors.

“Usually, in the last 48 to 72 hours (of a patient’s life), we do open that up for more family members to be there,” said Blackwood. “But this journey of end-of-life is long for some of our residents, and to not be able to have all their family surrounding them all the time has been difficult for us.”
These restrictions on visitors, though necessary for the safety of patients and staff, could be pushing people toward at-home hospice care rather than residential care if they have the choice.
Carol Seaby, executive director of the nursing agency At-Home Hospice in Ottawa, said she’s noticed a significant increase in interest in the at-home option.
“We’ve had many, many more requests for end-of-life at home, because when they go into a hospice institution they have restricted visiting as well as restricted hours,” Seaby said.
However, she noted that the reduced personal connection with PPE-clad caregivers has also affected care for at-home hospice workers, especially for their youngest patients.
“Children were more nervous about the masks,” said Seaby. “To have the nurse come in that they may have recognized for the last couple of years, and now it’s different, there has to be the comfort — you have to be able to do everything gently and nice.”
Having PPE essential
Seaby said they were fortunate to have adequate supplies and have worn full PPE since the beginning of the pandemic — something that is especially essential when caring for a patient who has COVID-19.
“If one of our clients was positive, we still provide care,” Seaby said. “We’re already in full protocol for it, but we’re aware… we follow the family through the course of it and make sure that all the contacts have been tested or at least aware if they’re visiting, we work inside their bubble with them.”
As COVID-19 has brought unprecedented issues into hospice care, the future is uncertain.
“It’s so hard to tell for the future, because I think most of these protocols are going to be in place for a while, probably until we have a cure or a vaccine,” said Blackwood.
Just as things were beginning to look up for greater normalcy in hospice care, Ottawa was turned into a red zone again in mid-October, rolling back to a modified Stage 2 level of reopening.
“We were starting to open things up, we were starting to bring in more volunteers, and we were thinking about day hospice and various things,” said Sullivan. “Now, for us, we’re stopping any expansion and closing down — making sure that we’re not introducing new people (such as administration staff).”
Ottawa’s COVID-19 second wave has also forced the organization to consider decreasing the number of essential visitors to fewer than three to lessen the chance of an outbreak.
Dr. Bellemare said he thinks once the pandemic is over and things go back to normal, the hospice community may retain certain practices learned during the pandemic.
“If those were beneficial changes to how they interact with the patients,” he said, “hopefully they will continue to employ them.”




